3 years after my last post, it seems this blog is in need of a sprucing up! There have been some big changes in my life since then, most notably that I somehow found my way back to academia (listen, I know I said "never" in my first post... but this is different!). I am currently finishing up my first year as an Assistant Professor on the tenure track at a small regional school, and while this past year was certainly no cake-walk (HyFlex teaching is hard, y'all!), I really, really love my new career. I love it so much in fact, that I want to learn everything I can about college science teaching and pedagogy. My hope is to share some of what I learn on this new adventure of mine right here on this blog. So stay tuned for some new directions here at the SciMinded Idealist! Right after I get through finals week...
Wednesday, May 5, 2021
Wednesday, May 2, 2018
Lung tumors "talk" to bone cells to promote tumor growth and spread!
And I'm back! My apologies for the long wait between posts; I've been working on a few other projects in the interim (more on this another time) and haven't had much time to write lately.
Anyway, let's dive right into the interesting science I have for you today! I'm jumping the gun a bit and posting this write-up of an upcoming episode of Audiommunity for two reasons, 1.) because we actually recorded the episode many months ago but had to painstakingly reconstruct the audio because of technical issues with our recording software, and therefore I have been sitting on this write-up for quite some time, and 2.) I just think this work is so darn cool!
In the general field of cancer research, the tissues, cells and organs directly surrounding tumors are referred to as the tumor "microenvironment", and understandably is a hot area of study. Having a good grasp on what the non-tumor "bystander" cells are doing near the tumor helps researchers develop better-targeted therapies (ie turning the immune system against the tumor, à la immunotherapy). But what is less well understood is whether or not tumors have any systemic effects on organs and tissues more distant from the primary cancer site, and whether those distant tissues may in turn influence the tumors growth and behavior.
To get at this question, Audiommunity's very own Camilla Engblom, along with coauthor Christine Pfirschke, and a large team directed by Mikael Pittet at Mass General Hospital in Boston, investigated a specific type of lung cancer called lung adenocarcinoma and discovered that, remarkably, the tumors "talk" to cells in the bone marrow (in mice). The result of this cross-talk is the trafficking of cells to the lungs that promote tumor growth and spread. This work was published in the journal Science last December as a paper entitled "Osteoblasts remotely supply lung tumors with cancer-promoting SiglecFhigh neutrophils".
So how did they make this important discovery? It began with a simple observation that mice with lung tumors had increased bone density and bone formation activity. They pinned that activity down to cells called osteoblasts, the cells in the bone marrow responsible for building new bone. To test the connection between the lung tumors and osteoblasts, they created a mouse model in which the osteoblasts were fluorescently labeled (so they could be tracked) and were able to be depleted in the mouse upon injection of diphtheria toxin. When they knocked down the osteoblasts in mice with lung tumors, they found that over time the tumors were reduced in size and number.
How were these bone marrow-resident osteoblasts having an impact on tumors all the way in the lung? The researchers hypothesized that the osteoblasts must be supplying the tumor microenvironment with tumor-promoting cells. When they looked at the type and amount of immune cell infiltrates in the lung, they found that knocking out osteoblasts resulted in a two-fold decrease of neutrophils. Coming at it another way, if they knocked down neutrophils using an antibody without knocking down osteoblasts, they saw a large reduction in tumor volume.
These results weren't associated with all neutrophils, but specifically a population of tumor-promoting neutrophils with high levels of a lectin called SiglecF on their surface. These SiglecF(high) neutrophils were pretty rare in normal, healthy lung tissue, but were increased 70-fold in mice with lung tumors! Differential gene expression comparing SiglecF(high) neutrophils to SiglecF(low) neutrophils showed the SiglecF(high) cells expressed genes associated with tumor-promoting functions, such as angiogenesis, myeloid cell differentiation and recruitment, extracellular matrix remodeling, suppression of T cell responses, and tumor cell proliferations and growth, among other things (yikes!). Additionally, when SiglecF(high) and (low) neutrophils were isolated from mice, mixed with lung tumor cells ex vivo, and then injected into new mice, tumor growth was accelerated in the mice that were injected with the SiglecF(high) neutrophil tumor preparations. So, clearly, SiglecF(high) neutrophils= bad news.
The final piece of the puzzle is figuring out how the tumor cells are communicating with osteoblasts in the bone marrow. A look at the serum from mice with and without tumors identified a candidate factor called RAGE (receptor for advanced glycation end products) that was upregulated about two-fold in the tumor-bearing mice. RAGE, as well as the circulating form of this receptor called sRAGE, have previously been shown to be connected with bone activity and regulation. In good agreement with this, when they added sRAGE to the serum of tumor-free mice, they saw increased osteoblast activity and increased bone marrow neutrophil maturation. While this part of the study will require more work to pin down, it all hangs together very nicely so far.
To summarize, lung tumor cells "talk" to bone marrow osteoblasts (possibly through a circulating factor called sRAGE), which then send tumor-promoting neutrophils to the sites of lung tumors. So what is the takeaway from this work? First, that osteoblast cell activity and SiglecF(high) neutrophils may be useful biomarkers in human patients, and possibly even good targets for cancer therapies. And second, and perhaps more importantly, that it is critical to consider the entire body when studying cancer because cancer is a systemic disease!
Nice work Camilla et al! Now please enjoy this cartoon!
Anyway, let's dive right into the interesting science I have for you today! I'm jumping the gun a bit and posting this write-up of an upcoming episode of Audiommunity for two reasons, 1.) because we actually recorded the episode many months ago but had to painstakingly reconstruct the audio because of technical issues with our recording software, and therefore I have been sitting on this write-up for quite some time, and 2.) I just think this work is so darn cool!
In the general field of cancer research, the tissues, cells and organs directly surrounding tumors are referred to as the tumor "microenvironment", and understandably is a hot area of study. Having a good grasp on what the non-tumor "bystander" cells are doing near the tumor helps researchers develop better-targeted therapies (ie turning the immune system against the tumor, à la immunotherapy). But what is less well understood is whether or not tumors have any systemic effects on organs and tissues more distant from the primary cancer site, and whether those distant tissues may in turn influence the tumors growth and behavior.
To get at this question, Audiommunity's very own Camilla Engblom, along with coauthor Christine Pfirschke, and a large team directed by Mikael Pittet at Mass General Hospital in Boston, investigated a specific type of lung cancer called lung adenocarcinoma and discovered that, remarkably, the tumors "talk" to cells in the bone marrow (in mice). The result of this cross-talk is the trafficking of cells to the lungs that promote tumor growth and spread. This work was published in the journal Science last December as a paper entitled "Osteoblasts remotely supply lung tumors with cancer-promoting SiglecFhigh neutrophils".
So how did they make this important discovery? It began with a simple observation that mice with lung tumors had increased bone density and bone formation activity. They pinned that activity down to cells called osteoblasts, the cells in the bone marrow responsible for building new bone. To test the connection between the lung tumors and osteoblasts, they created a mouse model in which the osteoblasts were fluorescently labeled (so they could be tracked) and were able to be depleted in the mouse upon injection of diphtheria toxin. When they knocked down the osteoblasts in mice with lung tumors, they found that over time the tumors were reduced in size and number.
How were these bone marrow-resident osteoblasts having an impact on tumors all the way in the lung? The researchers hypothesized that the osteoblasts must be supplying the tumor microenvironment with tumor-promoting cells. When they looked at the type and amount of immune cell infiltrates in the lung, they found that knocking out osteoblasts resulted in a two-fold decrease of neutrophils. Coming at it another way, if they knocked down neutrophils using an antibody without knocking down osteoblasts, they saw a large reduction in tumor volume.
These results weren't associated with all neutrophils, but specifically a population of tumor-promoting neutrophils with high levels of a lectin called SiglecF on their surface. These SiglecF(high) neutrophils were pretty rare in normal, healthy lung tissue, but were increased 70-fold in mice with lung tumors! Differential gene expression comparing SiglecF(high) neutrophils to SiglecF(low) neutrophils showed the SiglecF(high) cells expressed genes associated with tumor-promoting functions, such as angiogenesis, myeloid cell differentiation and recruitment, extracellular matrix remodeling, suppression of T cell responses, and tumor cell proliferations and growth, among other things (yikes!). Additionally, when SiglecF(high) and (low) neutrophils were isolated from mice, mixed with lung tumor cells ex vivo, and then injected into new mice, tumor growth was accelerated in the mice that were injected with the SiglecF(high) neutrophil tumor preparations. So, clearly, SiglecF(high) neutrophils= bad news.
The final piece of the puzzle is figuring out how the tumor cells are communicating with osteoblasts in the bone marrow. A look at the serum from mice with and without tumors identified a candidate factor called RAGE (receptor for advanced glycation end products) that was upregulated about two-fold in the tumor-bearing mice. RAGE, as well as the circulating form of this receptor called sRAGE, have previously been shown to be connected with bone activity and regulation. In good agreement with this, when they added sRAGE to the serum of tumor-free mice, they saw increased osteoblast activity and increased bone marrow neutrophil maturation. While this part of the study will require more work to pin down, it all hangs together very nicely so far.
To summarize, lung tumor cells "talk" to bone marrow osteoblasts (possibly through a circulating factor called sRAGE), which then send tumor-promoting neutrophils to the sites of lung tumors. So what is the takeaway from this work? First, that osteoblast cell activity and SiglecF(high) neutrophils may be useful biomarkers in human patients, and possibly even good targets for cancer therapies. And second, and perhaps more importantly, that it is critical to consider the entire body when studying cancer because cancer is a systemic disease!
Nice work Camilla et al! Now please enjoy this cartoon!
 |
| Hmm, this call seems legit... |
Monday, January 8, 2018
A vaccine for the common cold? Yes, please!
Happy New Year! This post is a few weeks overdue- my apologies! Blame it on the cold that keeps cycling through my family this month. Anyway, here we go:
Well folks, it’s that time
of year again. Snow is falling softly
from the sky, soup is bubbling on the stove, cookies are baking in the oven,
and my children are… oh god, my children are sick. Again.
In fact, they are on their second cold since November, and for the life
of me I cannot keep enough tissues on hand for their little, runny noses. And I, too, am on my second cold, and
positively drowning myself in Chamomile tea.
At night, I’m nestled in my bed (thanks to NyQuil) while visions of
cough drops dance through my head.
And I. Am. Miserable. I cannot
overstate this. All day long my head
hurts and my sinuses ache. My ears feel
like they might burst and my nose alternates between dripping like a faucet and
stopping up so tight I can’t breathe. I
cough so much my stomach muscles are looking like I’ve spent the last month
doing crunches (hey, silver linings, right?).
And if I am lucky, I will be out of the woods on this one in, oh, about
5-7 more days. Woof. And at the rate we’re going this year, I
might get two weeks of relatively healthy airways before I am taken down again
by the next cold virus that happens along.
This time of year I turn
into a real germaphobe (oh, who am I kidding?
I am a germaphobe all year). I
wash my hands so often they get chapped.
I ramp up the disinfecting of door handles, computer keyboards, and
light switches. I see germs everywhere I
look. The library. The grocery store. My son’s soccer games. My husband and children’s very
existence. I spend the months from
October to April just crossing my fingers and steeling myself against illness,
knowing that the name of the game is ugly survival. Because no one likes having a cold. At best, they are inconvenient and annoying,
and at worst they can put you out of commission for several days, exacerbating
chronic conditions like asthma and COPD, and landing you in the hospital with
pneumonia.
But researchers are fighting back by trying to create a vaccine for the common cold. Sounds simple, right? I mean we have vaccines for practically
everything else, so you are probably asking yourself, why don’t we have one
that works against colds? There are
actually a few good reasons we don’t yet have one.
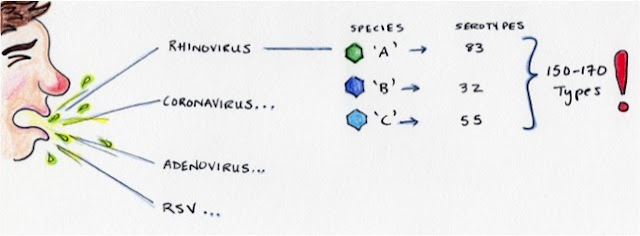
First of all, the common
cold is caused by a few different types of viruses, including but not limited
to rhinoviruses (the focus of this post), coronaviruses, adenoviruses, and respiratory syncytial virus, among others. Among the
rhinoviruses alone, there are 3 species (‘A’, ‘B’ and ‘C’) encompassing about
150-170 different strains that you can become infected with! We call these different strains
‘serotypes’. That is a lot of different viruses to vaccinate against.
Many of the established vaccines
that we receive protect against a single serotype of a particular
virus (ex the measles vaccine), or just a small number of serotypes (like the oral
poliovirus vaccine, which protects against all three serotypes of poliovirus). But the newer pneumococcal vaccine protects against 23 serotypes of virus! Vaccines that are able to
protect against multiple strains of a virus are called polyvalent vaccines, and researchers from Emory University School
of Medicine in Atlanta, Georgia, are trying to create a polyvalent vaccine that
would protect us against as many strains of the rhinovirus as possible.
On the most recent episode of
‘Audiommunity’ (Episode 27- Macaque PrisonGangs) we discussed a paper from this group at Emory entitled “A polyvalent
inactivated rhinovirus vaccine is broadly immunogenic in rhesus macaques”, which
was recently published in the journal Nature (read the original paper here). To briefly summarize the work, the
researchers made polyvalent rhinovirus vaccines by simply combining several
serotypes of rhinovirus together into a vaccine cocktail, and inactivating them
(so this is a “dead” vaccine, no live virus).
They then tested whether or not the cocktails could produce an immune
response in mice, and later, in rhesus macaques.
 |
| Different serotypes are mixed and inactivated with formalin |
The way they tested the
immune response to the vaccine was by injecting it into mice and then taking a
sample of the mouse serum and looking for “neutralizing antibodies”, against
each of the strains of rhinovirus in the vaccine. Neutralizing antibodies are proteins that are
made by our B cells that are designed to recognize an “intruder” (in this case,
the dead viruses in the vaccine), bind to it, and “neutralize” its biological
effects. A good vaccine should induce a
broad neutralizing antibody response, meaning that a lot of neutralizing
antibodies should be generated that recognize a lot of different parts of the
“intruder”.
 |
| Mouse is injected, serum is collected, and neutralizing antibodies measured |
What they found was that as
long as the input amount of viruses in the cocktail was high enough (we call
this the viral titer), they could get a decent immune response to the vaccine
no matter how many viruses they added to it (they tested 10-, 25-, and
50-valent vaccines in this paper).
Historically, two, 10-valent rhinovirus vaccines were tested in the
seventies that generated only a poor responses in test subjects (something like
only 30-40% of them). However, these
vaccines had really low input virus titers that were further diluted when made
into one-milliliter vaccine doses. The
researchers in this study recreated those vaccines using higher input virus titers,
and were able to improve the neutralizing antibody response significantly over
that of the original low titer vaccines.
 |
| The higher the input titer, the better the neutralizing antibody levels (inset: think of titer as concentration of viruses) |
They went on to test a
25-valent and a 50-valent vaccine in rhesus macaques, which are a nonhuman
primate common in medical research.
Remarkably, they were able to detect high levels of neutralizing
antibodies against 100% of the rhinovirus serotypes in the 25-valent vaccine,
and against 98% of the serotypes in the 50-valent vaccine! This is good news for humans, since the more
serotypes we can squeeze into the vaccine, the lower our chances of getting
sick become.
However, there are a few minor drawbacks to this work. The researchers found that the neutralizing
antibody response is serotype-specific; there is no
cross-neutralization against other viral strains not a part of a particular
vaccine. This means that an antibody against
one serotype of rhinovirus is not protective against a different serotype of
rhinovirus, so any serotypes not represented in a vaccine are still capable of infecting you and making you ill.
Another issue is that there were no challenge experiments in this
study. The reason for this is that there
are no animal models for the common cold (you can only recapitulate some of the
pathology in mice and rhesus macaques), so there is no way of knowing from this
study whether these vaccines will actually prevent you from getting sick. But this shouldn’t be too difficult to test
in a clinical trial in human subjects since cold viruses aren’t all that
pathogenic.
But perhaps the biggest
drawback to this work is that the researchers only tested polyvalent vaccines
against the ‘A’ species of rhinovirus.
Rhinovirus A accounts for about 83 strains of virus; but B accounts for
32, and the newly discovered ‘C’ species accounts for 55 strains, which is not a
small number of viruses, all vying to infect us. The problem is that the ‘C’ species viruses
are really hard to grow in cell culture.
And as this study showed, the success of the vaccine is all about
getting nice, high, input virus titers.
So in the meantime, researchers are working on figuring out the best
ways to grow these strains so they can add them into the vaccine
cocktails.
Emory has optioned the
vaccine technology to a startup company called MeissaVaccines, Inc. They have just
received an SBIR (small business innovation research) grant from the National
Institutes of Health to develop an 83-valent human vaccine, so let’s wish them luck
in their efforts to make the common cold a thing of the past! I, for one, will happily volunteer as a human
test subject!
Friday, December 8, 2017
Bugs in your gut and cancer immunotherapy
Hello, hello! Do I still have any readers? I took a bit of a long hiatus, but I’m back
and hopefully I will be posting more regularly.
And I have some news! As of a few
weeks ago, I am one of the newest cohosts for the immunology podcast
“Audiommunity” (www.emmunity.org)! I am pretty excited to have this opportunity
to discuss all the latest innovations in immunology with a team of
Harvard-trained immunologists. Of
course, I am not a Harvard-trained
immunologist, but I’m hoping I can add some value to the podcast by being
willing to ask the “stupid” questions (there are no stupid questions,
amirite?). I am also hoping to use my
blog space to distill some of the high-level research we will be discussing
into slightly more accessible summaries.
So if you don’t know one single thing about cancer immunology or
immunotherapy, I want you to be able to come away from my page with some new
knowledge.
So, without further ado… On
the latest episode of “Audiommunity” (episode
26- Lies and Magic), we discussed a recent research article that looked at
how the human gut microbiome might play a role in how well a patient with
metastatic melanoma responds to immune checkpoint blockade therapy (check
out the paper here). Okay, lots of
big terms in that last sentence, so let’s break it all down slowly:
 |
| "So, Doc, see anything in there?" |
First, let’s talk about the
microbiome. The microbiome is a
collection of genes from all the microbes (ie bacteria, fungi and viruses) that
live in and on us. As you have probably
heard, human beings are absolutely covered, head-to-toe and inside-out, with bacteria. They are on our skin, in our mouths, and,
yes, in our guts. At one time, it was
commonly believed that there are more bacterial cells on and in our bodies than
human cells, although the most recent estimates put that number closer to
one-to-one (read
more here). Still, that’s a lot of
bacteria (something like 30 trillion cells!).
We call these communities of bacteria the human microbiota, or the
normal “flora” (or as I like to call it, your “gut garden”, heh).
Metastatic melanoma, or
stage IV melanoma, is a truly horrible diagnosis to receive. It is melanoma (skin cancer) that has spread
through the lymph nodes to other areas of the body, most frequently the brain,
bones, lungs and liver. The 5-year
survival rate, which is the percentage of patients likely to be alive 5-years
after diagnosis, is very low, hovering around 15 to 20% (see
stats here). But recent, exciting
developments in cancer treatment are beginning to improve those odds, for
melanoma and other cancers. These new
treatments are called immune checkpoint blockade, or simply immunotherapy.
 |
| Seems legit. |
Cancer cells and tumors are
very tricky things. Since they are just our
own cells, gone wild, they can hold up signs that tell the cells of your immune
system not to attack. Normally, this is
a mechanism that healthy cells use to prevent things like autoimmune reactions
or to ramp down an immune response after an infection has been cleared. But
when used by cancer cells, this trick becomes a dangerous weapon in a tumor’s
arsenal.
The
way this works is the cancer cells express proteins on their surface that bind
to proteins on the surface of things like T cells, for example, and these
binding events cause the T cells to “shut down”. One of the proteins that these
cancers can express is called PD-L1 (for “Programmed cell death ligand-1), and
this binds to a protein called PD-1 (“Programmed cell death-1) on the surface
of T cells (click
here for a brief overview from the American Cancer Society).
The idea behind immunotherapy is to block
this binding event, so that the immune cells can raise the alarm against the
cancer and attack it. Scientists like to
refer to this as “taking the brakes off the immune system”. There are now antibody therapies that can
block both PD-L1 and PD-1 (for example, you may have seen TV ads for Merck’s Keytruda®,
also called pembrolizumab, a PD-1 inhibitor, and made famous by Jimmy
Carter), and these are turning out to be remarkably effective against many
different types of cancers (2012 NEJM
article).
But despite these advances,
sometimes immunotherapies don’t work well in some patients or for some types of
cancers, or
the improvements don’t last,
and no one really understands why. So in
the paper we discussed on Audiommunity this week, the authors set out to try
and discover whether the gut bacteria in melanoma patients receiving anti-PD-1
treatments had an effect on how well they responded to the treatments.
Outline of the study:
The researchers assembled a
group of patients with metastatic melanoma (they started with 112), and they collected
blood samples and tumor biopsies, and mouth swabs and stool samples to compare
the collections of bacteria in the guts of these patients. They used a technique called 16S rRNA
sequencing to determine which bacteria were present in the samples. 16S rRNA is a gene that all bacteria have (we
say that it is “well-conserved”), but it differs just a bit between different
species of bacteria, so it can act as a sort of molecular nametag for each of
the bugs that are present. The patients then received anti-PD-1 immunotherapy. And 6 months later, the researchers collected
samples again, determined whether patients had any improvement in their disease
(whether they responded to treatment), and repeated bacterial sequencing.
Results of the study:
What they found was that
patients that had a higher diversity of bacteria in their guts (more species,
or different types, of bacteria) did better with the treatment than patients
with less diversity. This isn’t a
surprising result, since it is pretty well known that loss of microbial
diversity, a condition called dysbiosis, results from, or causes, many types of
chronic diseases, including cancer (reviewed here).
They also found that patients with
specific types of bacteria had different treatment outcomes. Patients with higher levels of a genus of bacterium
called Faecalibacterium responded
better, whereas patients with higher levels of members of the order Bacteroidales
did worse.
 |
| Left gut: highly diverse, lots of multi-colored "sprinkles" (bacteria). Right gut: less diverse, fewer "sprinkles". |
Looking at the data a
different way, they found that they could predict which patients responded well
to the therapy just by looking at the composition of their gut bacteria. This is a potentially very useful tool for
the clinic, because being able to quickly and easily predict how well a patient
will do on a specific type of therapy before even beginning the treatment may save
critical time in the course of the cancer.
The researchers also compared
the types and numbers of immune cells and markers of immune system activation
both around the tumors themselves (the tumor microenvironment), and within the
gut. They found that in general there
were higher levels of things like tumor-killing T cells and inflammatory
markers in the patients that responded well to treatment, and higher levels of
suppressive immune cells in the patients that responded poorly. However, it is unclear whether the gut bacteria
directly led to these particular immune conditions or if this is just an
association.
Now this is where the study
gets really interesting (in my humble opinion).
They took stool samples from the patients, post-treatment, and
transferred them into “germ-free mice”.
These are mice that are born and raised in a sterile environment so that
they are not colonized by any microbes; this allows researchers to introduce selected
bugs into these mice to study their influence on things like the immune system.
After the transplant the mice now mirrored
their human patient counterparts (bacterially speaking). The mice were then injected with melanoma and
given immunotherapy. The mice that
received stool from patients that saw improvement in their disease in the
initial study wound up with much smaller tumors and higher levels of
tumor-fighting immune cells than the mice that received transplants from the patients
who didn’t improve. To put it more
plainly, the bacteria in the poop from patients that had a good response to
treatment seemed to help the mice respond well to treatment, too. Pretty cool, if you ask me!
The take-home message:
The long and short of it is
this; specific gut bacteria can affect the way a cancer patient responds to
immunotherapy. What is exciting about
this is that you can alter your gut microbiota through diet and exercise,
probiotics and antibiotics, and through stool transplants (which are already in
use in some diseases like Clostridium
difficile infection (CDI), to good effect). This means that it's possible that just some simple tweaks to the bacterial composition of your gut may make immunotherapy even more effective, and the authors of this study are already
designing a clinical trial that combines immunotherapy with microbiome alteration
(according
to this press release). However,
it is important to be clear that despite these promising results, patients
should not try to treat themselves with things like probiotics without the
express permission of their doctor (***I am not that kind of "doctor”, and
nothing in this article or on my blog should be taken as medical advice!!).
So that's all for now, folks. Please feel free to send me questions, and check back in about a week for my next summary!
Additional Note: the images featured in this post are my own, hand-drawn, mixed-media creations!
So that's all for now, folks. Please feel free to send me questions, and check back in about a week for my next summary!
Additional Note: the images featured in this post are my own, hand-drawn, mixed-media creations!
Paper reference:
V. Gopalakrishnan,
C. N. Spencer, L. Nezi, A. Reuben, M. C. Andrews, T. V. Karpinets, P. A.
Prieto, D. Vicente, K. Hoffman, S. C. Wei, A. P. Cogdill, L. Zhao, C. W.
Hudgens, D. S. Hutchinson, T. Manzo, M. Petaccia de Macedo, T. Cotechini, T.
Kumar, W. S. Chen, S. M. Reddy, R. Szczepaniak Sloane, J. Galloway-Pena, H.
Jiang, P. L. Chen, E. J. Shpall, K. Rezvani, A. M. Alousi, R. F. Chemaly, S.
Shelburne, L. M. Vence, P. C. Okhuysen, V. B. Jensen, A. G. Swennes, F.
McAllister, E. Marcelo Riquelme Sanchez, Y. Zhang, E. Le Chatelier, L.
Zitvogel, N. Pons, J. L. Austin-Breneman, L. E. Haydu, E. M. Burton, J. M.
Gardner, E. Sirmans, J. Hu, A. J. Lazar, T. Tsujikawa, A. Diab, H. Tawbi, I. C.
Glitza, W. J. Hwu, S. P. Patel, S. E. Woodman, R. N. Amaria, M. A. Davies, J.
E. Gershenwald, P. Hwu, J. E. Lee, J. Zhang, L. M. Coussens, Z. A. Cooper, P.
A. Futreal, C. R. Daniel, N. J. Ajami, J. F. Petrosino, M. T. Tetzlaff, P.
Sharma, J. P. Allison, R. R. Jenq, J. A. Wargo
Gut microbiome modulates response to anti–PD-1 immunotherapy in melanoma
patients. Science, 2017 DOI:
10.1126/science.aan4236
Thursday, March 16, 2017
Echoes of the bench in my everyday life
 | |
| Luggage tag I got from a vendor show. Free stuff! Yay! |
I have been a stay-at-home mom for 264 days, just a little under 9 months, and this is the longest I've been away from a lab in nearly 12 years. But who's counting? I am often asked by my friends still on the inside whether or not I miss the lab. The answer is a complicated one, rooted in practical forward-thinking optimism, but tinged with sappy nostalgia for the thing I spent the entirety of my twenties doing. Let me try to paint a picture for you of what it feels like to be a former bench jockey who finds herself exiled to Elba suburbia.
The closest I get to a centrifuge these days is the shiny, new, high-efficiency washing machine my landlord installed for us. Sometimes when I'm in my laundry room sorting grungy, stinky little boy clothes (oh, who are we kidding, my husband is an adult), I close my eyes and listen as the spin cycle revs up, the machine shaking ever so slightly as it cruises past 500 rpms, and I remember. I remember popping tubes into the centrifuge we called "the spaceship", a galactic-gray, futuristic monstrosity from the seventies. I had to use all my weight to latch the door. Then I would push "start" and back way, way up as it got up to speed, howling like a spaceship blasting off (hence the name), wondering all the while if this would be the time it finally failed and threw the rotor at me.
I open my kitchen cabinets to pull ingredients for dinner and suddenly I'm whisked back in time to the stock room at my last job; a walk-in closet of consumables and reagents, a science convenience store, if you will. The possibilities felt endless standing there inside that room, smelling of LB broth, the freshly cleaned glassware sparkling from it's shelves where it had been neatly put away according to size and category. A hyper-organized Type A's dream. Back in the present, I cast a resentful look at my sink full of dishes and remember the carefree joy of placing dishes in a tub near my bench, only for them to disappear and magically reappear hours later, clean and ready to use again. Maybe I should hire a technician? No, a housekeeping service. Well, we don't have the grant money for that anyway.
Later, after I've served a meal to my family who seemed only moderately impressed with my efforts and presentation, I am reminded of the many bosses, committees and reviewers that have judged my work, detached from the blood, sweat and tears I put into it. As I did back then, I will swallow my pride, take my critiques, and get back to it again tomorrow. Of course the one reviewer who was unnecessarily cruel will stick with me for a while ("that Western Blot was disgusting Mommy", or did my son say, "casserole"??...). I aliquot the leftovers and put them in the 4 degree freezer.
I wield wooden spoons and measuring cups like I once wielded pipets. I read cookbooks like I once read protocols, mixing and matching steps from several versions to come up with the best possible recipe. I occasionally explode things in the microwave, so that hasn't changed. I wear disposable gloves to cut up raw meat at BSL-1 and wonder to myself, "shouldn't I be doing this in the hood?".
I trade the latest news on childhood obesity and brain development with my children's pediatrician. We commiserate on the sinking vaccination rates and the latest outbreaks of things like the measles. We express our amazement at the newest recommendations for preventing peanut allergies (news flash: feed your baby peanut-containing products as early as 6 months- check out a piece I wrote for Scientific American Food Matters Blog for more on this). It's just like being back in the break room at work. The only things missing are some snacks pilfered from a random seminar and a good cup of coffee. Perhaps for my kid's next checkup I'll bring some Dunkins and ask the receptionist to babysit for a few minutes.
I read reviews of a new sippy cup I'm thinking of trying out on my toddler, and see advertisements that scream, "revolutionary design, strongest suction!" Of course I think, "show me the evidence! Where are the links to the data? And is 'strongest suction' really the best thing, physiologically, for the child? Perhaps a more moderate suction would be more beneficial to the development of their cheek and tongue muscles. And this cup is so new, it's barely made it beyond peer-review. Only 23 citations on Amazon..."
 | |
| This turkey is precisely 165 deg F (and only a little bit dry). |
Perhaps more practically, I clean my bathrooms with ammonia and worry about the development of resistant bacteria. I use a meat thermometer religiously (and frequently serve dried out, overcooked meat as a result) and worry about E. coli, listeria, and salmonella infections. I help my kids blow their noses and then immediately scrub my hands, hyper-aware of my fingers and keeping them away from my face.
At the same time, I don't stress out about mopping my floors regularly, knowing that a little household dirt is doing wonders to train my kid's burgeoning immune systems (what an awesome excuse to be a lazy housekeeper!).
My kids and I discuss science and medicine around the dinner table and on long car rides, and I supply answers to questions like, "why is blood red?" and " why is pee yellow?" and even "ewww! why does baby sister have blueberries in her poop?!" (kids are preoccupied with bodily fluids).
At the same time, I don't stress out about mopping my floors regularly, knowing that a little household dirt is doing wonders to train my kid's burgeoning immune systems (what an awesome excuse to be a lazy housekeeper!).
My kids and I discuss science and medicine around the dinner table and on long car rides, and I supply answers to questions like, "why is blood red?" and " why is pee yellow?" and even "ewww! why does baby sister have blueberries in her poop?!" (kids are preoccupied with bodily fluids).
In short, science has colored every aspect of my life. Being a scientist is as much a part of who I am as anything else that describes me is (ex "germaphobic", heh). I will always be a scientist in the way I act, think and feel, regardless of whether or not I suit up to go to work in a lab everyday.
So, do I miss working in a lab? Yes, I do. At least, I miss the idea of it, in the wistful sort of way that you might remember a time in your life that you didn't quite appreciate until it was over. But the things I learned from working in a lab come with me everyday in my life on the outside. And maybe, one day, I'll go back (although I've made certain friends promise to slap me if I ever seriously consider it), and bring some lessons I've learned on the outside with me. But that's a post for another time.
So, do I miss working in a lab? Yes, I do. At least, I miss the idea of it, in the wistful sort of way that you might remember a time in your life that you didn't quite appreciate until it was over. But the things I learned from working in a lab come with me everyday in my life on the outside. And maybe, one day, I'll go back (although I've made certain friends promise to slap me if I ever seriously consider it), and bring some lessons I've learned on the outside with me. But that's a post for another time.
Monday, January 9, 2017
DinoMania!
Happy New Year! This post was meant to go up a lot sooner (like, before Thanksgiving...heh), but well, holidays and kids and business and excuses, etc, etc. Anyway, without further ado- it's time for DinoMania!
When I was a kid, I loved
dinosaurs. ‘Love’ probably isn’t even a
strong enough word. I was infatuated with them. From the time I was about six years old, I
wanted to be a paleontologist when I grew up.
I checked out nearly every dinosaur book in the children’s section of
our small town library, and spent many, many weekends with my Dad at the Dinosaur State Park in Rocky Hill. Of course my favorite place to go was the Yale Peabody Museum in New Haven, where I
would wander the Great Hall of Dinosaurs and marvel at the massive brontosaurus
skeleton, trying to imagine what it would have been like to stand next to these
great and terrible lizards (dinosaur is Latin for “terrible lizard”).
Fortunately (or unfortunately),
when I was around eight years old, Steven Spielberg went right ahead and did
the imagining for me with a little movie called “Jurassic Park”, which
basically ruined dinosaurs for me forever.
To this day I can’t eat jello without scrutinizing it for a rhythmic
jiggle, indicating I’m about to be ambushed by a massive T. rex with a taste for man-flesh.
And let’s not forget that gratuitous doghouse-eating scene from one of the
horrifically bad sequels. Totally
unnecessary, Steven.
Rather than stoke my
interest in a particular career path, movies have kind of a history of turning
me off of a field. “Jurassic Park”
crushed my paleontology dreams. “Apollo
13” made me rethink my plans of becoming an astronaut- I didn’t think it was
possible to be any more emetophobic until I watched Bill Paxton puke in zero
gravity- thanks Ron Howard! My interest
in ancient civilizations? Destroyed by
nightmares after watching “The Mummy” in a hotel room on a rainy vacation to
Salem, Massachusetts around Halloween time.
Bad combination. Weirdly enough,
the movie “Outbreak” did not manage to scare me away from virology, and I
became a virologist anyway, but I digress.
The point is, don’t get your
career aspirations from movies. It’s
much better (and much more accurate and informative) to stick with books, obviously. Nice, safe, papery, books.
 |
| Cake that took me fifty million years to complete. |
In my house it seems that my
love of dinosaurs has not skipped a generation, and my four-year-old son owns
lots and lots of books about them. We just threw him a dinosaur-themed birthday
party a few months ago, and he loves to talk about dinosaurs for hours on end,
which isn’t all that unusual for children his age. In fact my husband and I have a theory that a
general fascination with dinosaurs is a normal developmental stage for all
mini-humans. Much like when I was a kid,
my son has read through practically the entire dinosaur section of our local
library, and anytime we are in the vicinity of our favorite Barnes and Noble we
somehow manage to return home with a new tome full of the beasts.
One book in particular, “PrehistoricPredators”, by Brian Switek, is our all-time favorite and I highly
recommend it to anyone who has a dino-loving child at home. The illustrations are beautiful, the facts
plentiful, and the pronunciation key is clutch.
My son’s obsession with this book has spawned his favorite,
self-invented game, which he has christened “the dinosaur game”. The idea is that you take turns going back
and forth naming dinosaurs until one person can no longer think of dinosaurs to
name. Sounds easy, but it turns out some
four year olds play for keeps.
Four year old: “Okay, I’ll go first. Diplodocus.”
Me: “Ummm, Tyrannosaurus rex”
Him: “Giganotosaurus”
Me: “Uh, velociraptor.”
Him: “Dilophosaurus.”
Me: “Dilopho…What? Uhhh, umm. Stega, uh, rapta… don.”
Him:
“Haha! Mommy! ‘Stegaraptadon’ is NOT a dinosaur. You just made that up! You could’ve said stegasaurus or dimetrodon.
Duh, silly! I win. Now I get ice cream!”
Sheesh. I didn’t realize there was ice cream at
stake. Silly me; ice cream is always at stake when you have a
preschooler around. Guess I should pay
more attention during story time.
 |
| The mighty Stegaraptadon. Totally real, I swear. |
 |
| Part of the collection. |
 |
| Image from Goodreads.com |
Well, speaking of story
time, I happened to be browsing the new nonfiction section of the library
recently when I stumbled upon an eye-catching title. “TheTyrannosaur Chronicles: the Biology of the Tyrant Dinosaur” by Dr. David Hone jumped out at me without
warning*. And I’m glad it snared me because it is a fantastically interesting
read for grown ups that never quite “grew out of” their dinosaur phase.
Dr. Hone has written a
comprehensive field guide about everyone’s favorite dinosaurs, the tyrannosaurs,
and contains beautiful illustrations and figures by Scott Hartman. Hone covers the history of the discovery of
the large family (yes, family- did you know that more than 30 species of
tyrannosaur has been discovered so far?), with the mighty T. rex being named in 1905. Tyrannosaurs first appeared in the
Jurassic period, but unlike the massive apex predator depicted in the infamous
film, the first tyrannosaurs were small, about the size of a horse. Over time the general trend was for tyrannosaurs
to get bigger, and eventually they did resemble the monster we now think of
when we think of T. rex.
But they may not have looked
so much like the scaly reptiles of our time.
It’s generally accepted that birds are the living descendants of
dinosaurs, having evolved from some avian theropod ancestor. Think chickens, not crocodiles. And man, do chickens creep me out- those ugly
feet! Those staring, unblinking eyes! As
far as I’m concerned, the resemblance to the terrible lizards is clear
(apologies to my Mother, the crazy chicken lady). And phylogenetically speaking, there is goodevidence to support this relationship.
Although tyrannosaurs themselves are probably more closely related to
crocodiles than the “bird-like” dinosaurs were, it is now believed that they
(as well as many other dinosaurs) were covered in a downy plumage, perhaps for
insulation and for attracting mates.
A few of my other favorite
tyrannosaur facts that I picked up from this book include that they had large
air spaces in their skulls and highly developed nasal cavities for smelling. And much like birds, tyrannosaur bones had
pneumatic air sacs that were filled by air from the lungs. In a section discussing the ecology of
tyrannosaurs, it is explained that far from modern imaginings of T. rex battling a triceratops,
tyrannosaurs actually battled each other both for sexual dominance and for food
(yep, they ate each other sometimes). And
they did far more chewing of their prey than wholesale “gulping”, as suggested
by the discovery of pulverized hadrosaur bones in fossilized tyrannosaur
droppings. Most of all, I was fascinated
to learn that it is incredibly difficult to determine the sex of a dinosaur
from its fossil, or whether a smallish fossil is a juvenile, an outlier, or a
new species entirely. It truly is a
remarkable researcher that can be satisfied working with such “bare
bones” (pun intended).
Overall, I enjoyed the book,
though at times it got fairly academic and may not be for the casual
reader. But if you loved dinosaurs as a
kid and you enjoy some pop-sci nonfiction, check out this book.
To wrap up this “dino-mania”
post, I just want to mention that it was reported recently in Current Biology that
a dinosaur tail covered in primitive plumage was discovered, preserved in amber
(here’s the link to a Sciencepiece about the article since the article itself is not open access). The images are beautiful, and although
dinosaur-era feathers preserved in amber are nothing new, this is the first
time a mummified piece of dinosaur skeleton and tissue has been found along
with the feathers. An actual dinosaur tail.
But before you start freaking out, thinking, “this is exactly how Jurassic Park got started!”
(I mean, I didn’t think that or anything…) it turns out that no dino DNA could
be recovered from the sample, so we’re still safe. For now.
*Note that they don’t allow
jello or other food in the library, even just to serve as an alarm against
imminent dinosaur attack (“No Ms. Librarian, I am not going to eat this jello,
I’m just going to stare at it to make sure it doesn’t start to jiggle…”).
Subscribe to:
Comments (Atom)